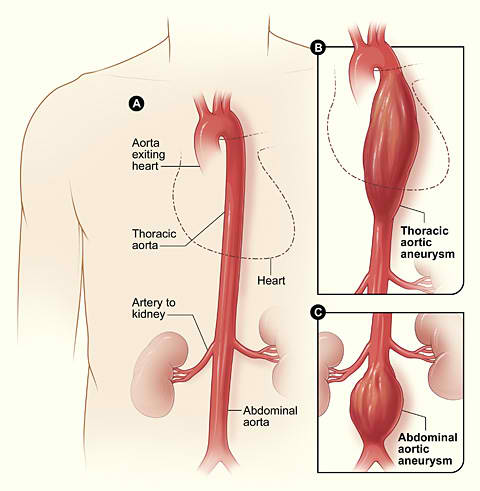
Aneurysms can affect any artery but most commonly affect the aorta. The aorta runs from the heart through the chest and abdomen and gives off several very important branches supplying all internal organs, the spinal cord and the lower limbs.
An aortic aneurysm can occur in the chest (thoracic aortic aneurysm) or the abdomen (abdominal aortic aneurysm).
WHY IS AORTIC AN ANEURYSM DANGEROUS?
The normal aorta measures around 15 to 20 mm in diameter and has a strong and healthy arterial wall to sustain high pressure. Aortic aneurysms cause weakness in the wall of the aorta and increase the risk of aortic rupture. The larger the aortic aneurysm the higher the chance of aorta bursting. When aneurysms rupture, blood suddenly escapes and this haemorrhage is life threatening. The consequences of aortic aneurysm rupture are disastrous and mortality is still between 50 to 70 %.
HOW CAN AN AORTIC ANEURYSM BE DIAGNOSED?
Aortic aneurysm is usually asymptomatic so patients are not aware of it. Men over 60 years are most frequently affected and those who have a positive family history may develop an aneurysm even earlier in life. An ultrasound scan is a reliable, pain free, quick and relatively inexpensive technique used to diagnose large aortic aneurysms. Ultrasound scans performed in a dedicated vascular laboratory is recommended for the above mentioned groups of patients.
HOW IS AN AORTIC ANEURYSM TREATED?
Every patient is unique and every aneurysm is different thus every case will be discussed with a consultant individually. In general, however, small aneurysms may be treated with medication and observation.
For larger or symptomatic aortic aneurysms several different treatment options exist:
Open aneurysm repair. Thoracic or abdominal aortic aneurysms can be repaired with a classical open surgical technique. This is a major procedure and the patient will be informed fully about all aspects. Also, in patients with other significant diseases there will be consultation with other specialists within our multidisciplinary team in order to deliver the best quality care.
Depending on the location of the aneurysm an incision will be placed over the tummy under general anaesthetic and the weakened aorta will be cut off and replaced with a synthetic tube graft. The patient stays in an Intensive Care Unit for the first several hours and then he/she will be transported back to their surgical department. The total hospital stay is usually one or two weeks.
Endovascular stent graft. This mini invasive, or keyhole, surgical procedure is mainly performed on patients who are medically not fit enough for open surgery. However, the patients may wish to have this procedure done even if they are fit for open surgery. The most important prerequisite is appropriate aortic anatomy. Everyone’s aorta will be thoroughly evaluated with a CAT scan or angiogram (dye test), measured and a custom made stent graft will be made for an individual patient if needed. The stent graft or endograft, will be introduced into the patient’s aorta using a catheter (a thin, flexible tube) inserted through a small incision into an artery in the groin. Under real-time x ray imaging the surgeon will guide the stent graft above and below the aneurysm and will exclude the weakened part of the patient’s aorta from the circulation.
General anaesthetic might still be required, but since the abdomen is not entered to accomplish the repair the patient usually leaves the hospital earlier then in the case of open aortic aneurysm repair. Postoperative follow up is necessary and CAT scan or ultrasound scans need to be done every year to make sure the stent graft is working well.